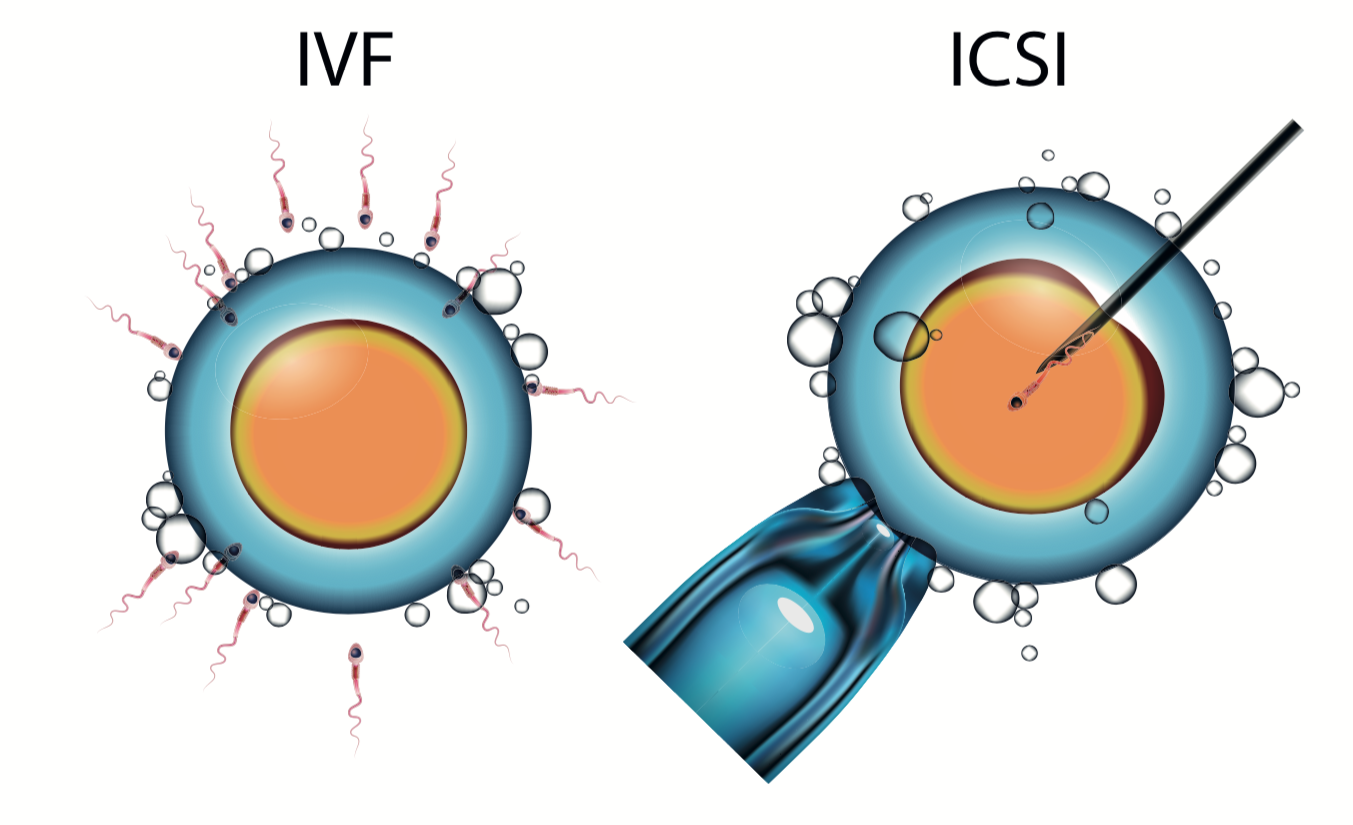
The end of the ‘test tube baby’ could be in sight after British doctors launched a new form IVF which allows conception to take place in the womb, like a natural pregnancy.
The technique, described as ‘a real breakthrough’ involves placing egg and sperm cells into a tiny silicone capsule, the size of a grain of rice, and inserting it into the womb.
Doctors say it gives couples a psychological boost, knowing that the child has actually been conceived inside the mother, while the embryos benefit from being in the perfect conditions for fertilisation. It contains 360 holes so fluid from the womb can surround the egg and sperm.
After 24 hours the capsule is removed and doctors select the most healthy embryos for implantation into the womb lining of the mother.
"The introduction of this device signals a real breakthrough in IVF treatment as it enables women to care for an embryo in its earliest stages of development for the first time,” said Professor Nick Macklon, medical director at Complete Fertility Centre Southampton, which is located within the city's Princess Anne Hospital, part of University Hospital Southampton NHS Foundation Trust.
"That is important psychologically as it involves parents-to-be directly with the fertilisation process and early embryo development but, perhaps more importantly, it also could provide many potential health benefits for babies born following fertility treatment."
The technique, which uses a tiny device called AneVivo, which is just 1cm long and 1mm wide.
Doctors are hoping the new technique will improve the health and weight of babies born through IVF.
"Babies born following IVF treatment have been shown to have lower than normal birth weight and, although not initially a problem, we know there is a link between low birth weight and long-term health and the laboratory environment could play a part in this,” added Prof Macklon.
"Through the use of AneVivo, in addition to the fact fertilisation takes place in the natural environment of the womb with access to nutrients and signals from the mother, we can reduce exposure to the synthetic culture fluids used in the laboratory and help to determine precisely what effect this may have."
Pascal Mock, the Swiss medical scientist who invented the device, said it gave couples greater dignity.
"In a normal pregnancy the embryo has very little contact with the environment and is less influenced by temperature, pressure and light,” he added
“The early embryos start life in close contact with the mother, recreating the two-way exchange of fluids during the early stages of its development."
Prof Macklon, who is also chairman in obstetrics and gynaecology at the University of Southampton, added: "This is a very significant moment in the advancement of fertility treatment in the UK and we are all extremely excited to be able to offer patients the option of a more natural fertilisation process."
Geoffrey Trew, consultant in Reproductive Medicine and Surgery at IVF Hammersmith said the technique was promising but needed real-world data to see if it turned out to be better than traditional lab fertilisation.“These techniques were first looked at a low tech way of introducing IVF into thid world countries where there are not the high tech labs with strict air quality available,” he said.
“The lab part in traditional IVF is high tech but may give better results - hence the development of time lapse incubators which may also allow the selection - more accurately - of the single embryo that is best to put back.
“So - promising - if used correctly - but more data needed to see real success rates and how they compare to 'traditional' lab work.”